Cavity Treatment
Understanding Cavities

Cavities occur when certain bacteria in your mouth, like mutans bacteria, use sugar to produce acid. This acid then dissolves the surface of your teeth, leading to tooth decay.
It's important to know that cavities cannot heal naturally and won't return to their original state on their own. That's why dental treatment is necessary. We treat cavities by carefully removing the decayed portion of the tooth and then restoring it with a filling or a crown to protect it.
The Cause of Cavities
The Three Key Factors in Cavity Formation
- Bacteria (Mutans Bacteria) Mutans bacteria are tiny, spherical bacteria, about 1 micrometer (1/1000th of a millimeter) in size. They attach to the surface of your teeth, forming plaque, and then produce acid from the sugars you consume. This acid dissolves the calcium and phosphorus in your teeth, making them weak and porous.
- Sugar (Carbohydrates) The sugars (carbohydrates) found in food, especially refined sugar, are what mutans bacteria use to create acid. If you snack frequently or regularly consume sweet treats like candies and sugary drinks, your tooth surfaces are exposed to acid for longer periods, which increases your risk of developing cavities.
- Tooth Quality Everyone's teeth are a little different due to factors during their development. Some people's tooth quality – the condition of their enamel and dentin – makes them more susceptible to cavities. This is especially true for children who have just gotten their baby teeth or new permanent teeth, so it's extra important to be mindful during these times.
When these three factors combine, cavities begin to form over time.
To help grow strong, healthy teeth, it's important to get the right nutrients. These include high-quality protein to build the tooth's foundation, calcium and phosphorus for tooth remineralization, and essential vitamins like Vitamins A, C, and D to help these minerals work effectively. Aim for a balanced diet to support your dental health!
Our Approach to Comfortable Treatment

At our clinic, we are dedicated to providing treatment that is as comfortable and pain-free as possible.
Anesthesia is used to minimize pain during procedures, but we understand that the injection itself—both when the needle goes in and when the anesthetic solution is administered—can cause discomfort.
- Topical Anesthesia: We apply a topical anesthetic beforehand to numb the area, significantly reducing the sensation when the injection needle is inserted.
- Electric Anesthesia Delivery: Pain during anesthetic solution injection often comes from inconsistent speed and pressure. To counter this, we use an electric anesthesia delivery system that ensures a steady, gentle flow.
- Minimizing Discomfort: We also use ultra-fine needles and warm the anesthetic solution to body temperature before injection. These various methods are all part of our commitment to reducing any discomfort you might feel.
That's why we take several steps to make your experience smoother:
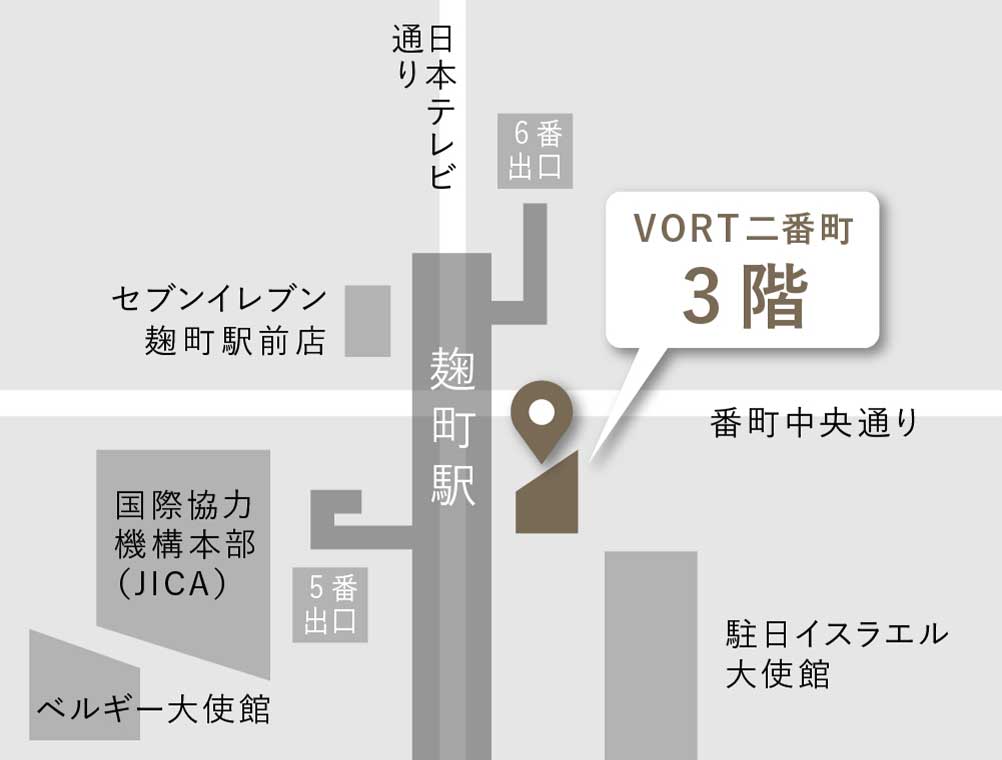
Understanding Cavity Stages and Treatment
-

CO stands for "Caries Observation," and it's professionally referred to as a tooth that needs observation. This is a very early stage of tooth decay where there isn't yet a visible hole in the tooth surface.
At this point, we can often encourage the tooth to remineralize (naturally strengthen itself) through good daily oral hygiene at home and fluoride application during your regular check-ups. We'll then monitor the tooth's progress. -

This stage of cavity involves the enamel, which is the outermost layer of your tooth. At this point, the enamel has just begun to dissolve.
We can usually treat this by gently removing a small amount of the affected tooth and then filling it with composite resin. Since the enamel doesn't have nerves, you typically won't feel any pain during this procedure. Composite resin (often abbreviated as CR) is a tooth-colored, plastic material. It's great because we can shape it precisely, meaning we need to remove very little of your natural tooth. Plus, the treatment can usually be completed in just one visit. -

This stage means the cavity has progressed past the enamel and reached the dentin, which is the layer just beneath it.
Because dentin is a softer tissue than enamel, cavities can spread more quickly once they reach this point. For these types of cavities, we might still use the composite resin (CR) filling mentioned earlier. However, depending on the size and location of the cavity, we may need to use an inlay or onlay (which are partial coverings) or even a full crown that completely covers the tooth.
While a CR filling can usually be completed in just one visit, if a partial or full covering is needed, it will require at least two visits. This is because we first prepare the tooth and take an impression for the custom-made restoration. Then, it takes approximately one to two weeks for the restoration to be crafted before you return for the final placement. -

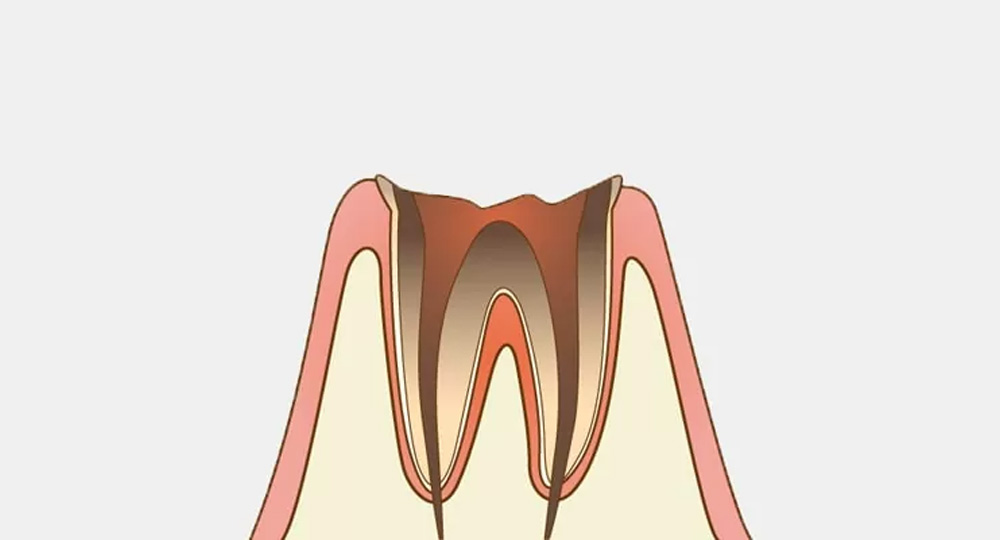
This is a more advanced stage where the cavity has reached the pulp, the innermost part of your tooth containing the nerves and blood vessels.
You might see a large hole in the tooth, or sometimes a seemingly small hole might hide extensive decay internally. When decay reaches this point, it often negatively impacts the tooth's nerve, and if inflammation occurs, it can cause severe pain. If the nerve is inflamed, we will need to perform root canal treatment (a procedure to remove the nerve).
If you're experiencing tooth pain without doing anything, or if hot or cold foods and drinks consistently cause pain, it might be necessary to have a root canal and have the nerve removed. During this procedure, we'll use local anesthetic, then gently remove the nerve using very fine, file-like instruments. After the nerve is removed, we sterilize the area and then fill the space with a special root canal filling material or medication to prevent re-infection.
Following the root canal, we'll build up the tooth's structure, take an impression for a crown, and then place the custom-made crown. This entire process typically takes about one month. A tooth that has had its nerve removed is called a "non-vital tooth" and becomes more brittle than a healthy tooth. The nerve plays a crucial role in delivering nutrients to the tooth, so once it's gone, the tooth cannot regenerate itself. Removing a tooth's nerve is a more significant decision than many people realize. -
At this advanced stage, most of the visible tooth structure is gone, leaving primarily the tooth root (the "root" of the tooth) remaining. When decay progresses this far, the tooth's nerve often dies, and you may even stop feeling pain directly from the tooth itself. However, you might experience pain due to pus accumulating around the root. Since oral bacteria can affect your overall health, we cannot leave this condition untreated.
Our first step is to assess if the remaining tooth structure can be saved. We'll check the size of the cavity and whether the remaining portion of the tooth is fractured. If it's salvageable, we'll proceed with treatment. Unfortunately, if the tooth is deemed too difficult to save, extraction (removing the tooth) will be necessary.
If extraction is required, we'll then discuss options to replace the lost tooth and restore its function. Dental implants, bridges, and dentures are common solutions. Regardless of the chosen option, we'll need to wait for the gum tissue to heal completely after the extraction. In the case of implants, a surgical procedure is also involved, so these processes can take some time.
CO: Initial Cavity
(Observation Needed)
C1: Cavity in the Enamel
C2: Cavity Reaching the Dentin
C3: Cavity Reaching the Nerve (Pulp)
C4: Extensive Tooth Loss
Cavity Prevention: Your Best Defense

Preventing cavities hinges on three crucial elements:
- Reducing cavity-causing bacteria.
- Limiting their activity.
- Strengthening your teeth.
The Importance of Brushing
Reducing cavity-causing bacteria primarily means removing plaque. Plaque is a sticky substance produced by these bacteria that adheres firmly to your teeth. It's so tenacious that rinsing alone won't remove it; you need to physically scrub it off with a toothbrush. This is why toothbrushing is the fundamental step in cavity prevention. The main goal of brushing is to remove plaque from the tooth surfaces, especially near the gum line.
Additionally, for cleaning between your teeth, you'll need dental floss or interdental brushes.
When to Brush Your Teeth
So, when is the best time to brush? Even if your meal doesn't contain obvious sugar, it still has carbohydrates that cavity-causing bacteria feed on. Once you eat, bacteria in plaque quickly take up these sugars and produce acid. Therefore, the basic rule is to brush immediately after meals. The same goes for snacks – "brush after you eat" is key.
However, brushing five or six times a day isn't realistic for most people. A practical brushing routine would be after breakfast, after lunch or a snack, and most importantly, before bed. Especially while you're sleeping, your body's functions slow down, and saliva flow decreases, creating an ideal environment for bacteria to thrive. Brushing thoroughly before bed to reduce bacteria is extremely effective.
Using toothpaste also helps remove stains more efficiently and keeps your teeth cleaner. Most toothpastes contain fluoride, which is effective in making your teeth more resistant to acid. Apply an appropriate amount of toothpaste, spread it over all your teeth, and then brush thoroughly. After brushing, spit out the toothpaste, but only rinse lightly, perhaps once. This allows fluoride and other tooth-strengthening and remineralizing agents to stay in your saliva longer.
Saliva is also excellent at washing away food debris in your mouth. To produce more saliva, it's important to chew your food thoroughly during meals. The action of chewing also helps clean the surfaces of your teeth. If you consistently eat soft foods without much chewing, plaque can remain attached to your teeth, allowing bacteria to continue multiplying.